Trigeminal Neuralgia
Trigeminal neuralgia causes sudden, electric shock-like facial pain triggered by simple actions like chewing or talking. It results from irritation of the trigeminal nerve, making daily life difficult. The IGNIte procedure offers a breakthrough, minimally invasive treatment that calms the nerve using your body’s own healing factors. Contact UsThe IGNIte Procedure
(Image-Guided Neurobiologic Injections)
Trigeminal neuralgia can feel overwhelming, but effective relief is within reach at CSC. Our targeted care combines state-of-the-art treatments like the IGNIte procedure with a compassionate approach tailored to your unique needs. Watch the adjacent video to discover how this innovative technique has transformed the lives of patients suffering from trigeminal neuralgia.
What Is the Trigeminal Nerve—and Why Does It Matter?
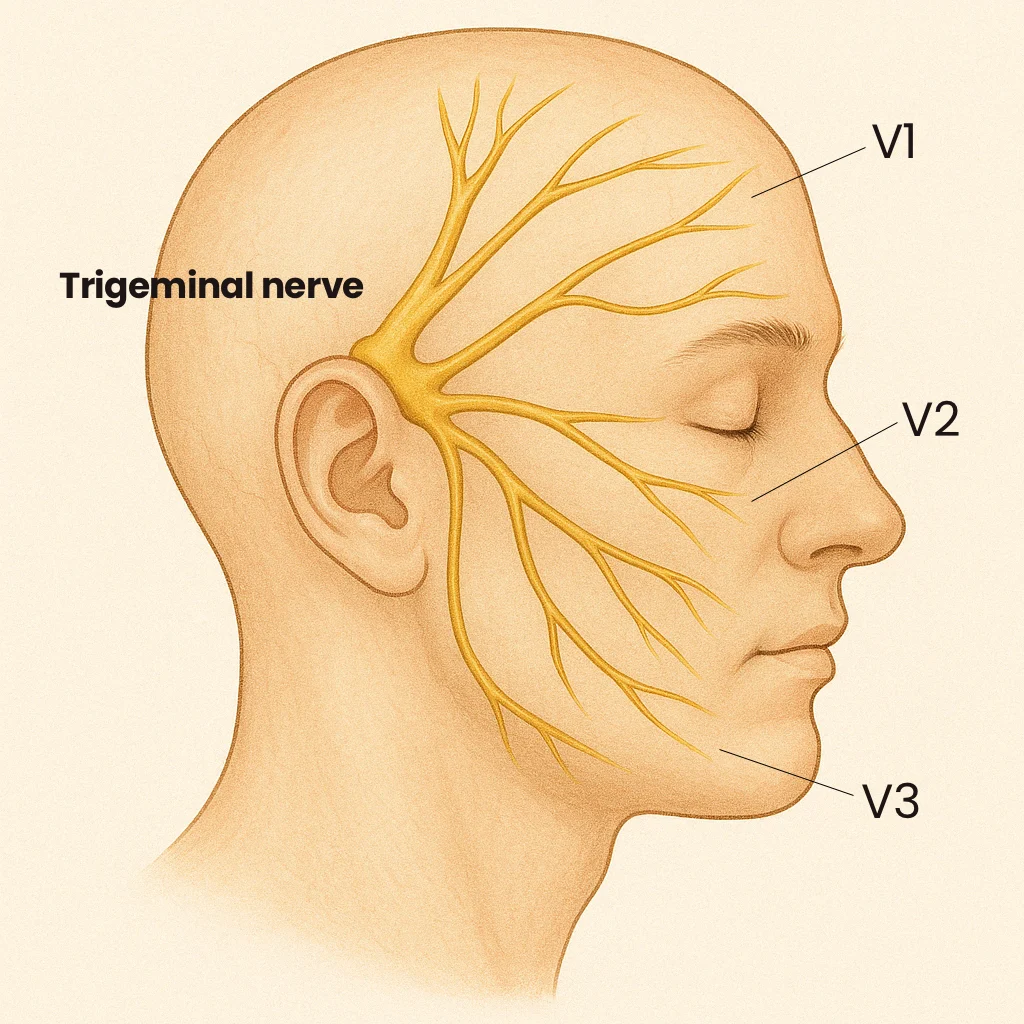
Think of the trigeminal nerve as your face’s main communication line—it’s how your brain feels and moves everything from your forehead to your jaw. It branches into three key parts:
- V1 (ophthalmic branch) handles signals from your forehead, eyes, and upper nose.
- V2 (maxillary branch) picks up sensations from your cheeks, upper jaw, and nasal cavity.
- V3 (mandibular branch) is the multitasker—unique among the branches, V3 carries both sensory and motor fibers. It supplies sensation to the lower jaw, teeth, and part of the tongue, while also powering the muscles involved in chewing and speaking.
When this nerve gets compressed or irritated—as in trigeminal neuralgia—it can cause sharp, electric shock-like pain that disrupts even the simplest movements.
Trigeminal Neuralgia (TN)
Trigeminal neuralgia is a nerve condition that causes sudden, intense facial pain—often triggered by simple things like talking, chewing, or even a light touch. This pain comes from irritation or pressure on the trigeminal nerve, which controls feeling in your face. It’s often caused by a nearby blood vessel pressing on the nerve, but can also be linked to aging or conditions like multiple sclerosis.
Many describe it as one of the most unbearable types of pain, making everyday life feel impossible. While medications and surgery can help some, new minimally invasive treatments are giving fresh hope to those who haven’t found relief with traditional options.
How to Recognize the Signs of Trigeminal Neuralgia
Trigeminal neuralgia (TN) comes with intense, sudden facial pain that can stop you in your tracks. The episodes are unpredictable, making it important to recognize the signs early so you can get the right help. While sharp, electric shock-like pain is the most well-known symptom, TN can show up in other ways too:
Pain while chewing or talking
Everyday activities like eating or speaking can trigger or worsen the pain, turning simple tasks into challenges.
Sudden, stabbing facial pain
The pain often feels like an electric jolt and typically hits the jaw, cheek, or eye area without warning.
One-sided pain
TN usually affects just one side of the face, depending on which part of the nerve is involved.
Brief attacks, often in bursts
Episodes may last only a few seconds, but they can come in waves throughout the day.
Burning between flare-ups
Some people feel a lingering burning or aching sensation between attacks, adding to the overall discomfort.
If you’re noticing these symptoms, especially recurring sharp pain in your face, it may be time to explore treatment options.
Common Causes Of Trigeminal Neuralgia
Nerve Damage
Damage to the trigeminal nerve is a primary cause of TN, disrupting its normal function and causing painful episodes.
Inferior Alveolar Nerve Injury
Inferior Alveolar Nerve Injury
This injury, often associated with dental procedures, is a common cause of TN affecting the V3 branch. For a detailed explanation, refer to the video above, which highlights how such injuries lead to this type of trigeminal neuralgia.
Tumors
Tumors near the trigeminal nerve can compress or damage the nerve, leading to persistent or progressive symptoms.
Physical Trauma
Head or facial trauma can injure the nerve, either directly or through swelling, resulting in neuralgia.
Anesthetic Injections
Improperly administered nerve blocks or local anesthetics can inadvertently damage the trigeminal nerve.
Endodontic Treatments
Root canal procedures, if complicated, may impact the nerve, particularly in the mandibular region.
Dental Surgical Procedures
Dental surgeries, such as extractions or implants, may inadvertently harm nearby nerve structures, potentially triggering TN.
Vascular Theory
An artery or vein may press against the trigeminal nerve near the pons or along its pathway. This can damage the protective myelin sheath and cause the nerve to malfunction, leading to sudden, intense nerve activity. Symptoms often appear in areas controlled by the V2 (middle face) or V3 (lower face) branches of the nerve.
When Do You Need To Seek Medical Help?
- Frequent or persistent facial pain that interferes with daily activities.
- Pain that no longer responds to typical medications or becomes refractory to treatment.
- Pain that radiates or spreads beyond the usual trigeminal nerve distribution.
How Trigeminal Neuralgia Is Accurately Diagnosed
Accurately diagnosing trigeminal neuralgia involves a combination of a thorough medical history, clinical examination, and advanced imaging techniques.
- Medical history and physical exam: A detailed review of symptoms helps identify patterns of pain characteristic of TN, such as triggers, duration, and localization.
- Neurological exam: Tests focus on assessing facial sensation, motor function, and reflexes to rule out other conditions.
- Magnetic resonance imaging (MRI): High-resolution MRI, sometimes with contrast, is used to detect vascular compression, tumors, or structural abnormalities affecting the trigeminal nerve.
- Diagnostic nerve blocks: Occasionally, a nerve block is performed to confirm the involvement of the trigeminal nerve in the pain pathway.
Finding Relief: Treatment Options for Trigeminal Neuralgia
If you’re living with the intense, electric shock-like pain of trigeminal neuralgia, you know how disruptive it can be. Many patients start with medications like carbamazepine or oxcarbazepine, which can help calm nerve activity. Others find some relief with nerve blocks, acupuncture, or short-term use of stronger pain medications—but these solutions don’t always last and can come with unwanted side effects.
IGNIte Procedure: A Safer Approach
At CSC, we’re proud to offer the IGNIte procedure, a groundbreaking, minimally invasive treatment designed to provide lasting relief from trigeminal neuralgia. Unlike traditional surgeries or radiation, the IGNIte procedure targets the root cause of your pain—calming the overactive trigeminal nerve—without harming surrounding tissues. This means quicker recovery, fewer risks, and a more effective solution for long-term relief.
Exclusively available at CSC, the IGNIte procedure utilizes advanced neurobiologics to precisely reduce nerve hyperactivity while preserving healthy structures. Performed by a board-certified specialist, this innovative approach minimizes downtime and avoids the complications typically associated with traditional treatments.
